Abdominal Aortic Aneurysm
The aorta is the largest artery in the body, responsible for distributing oxygenated blood to the rest of the circulatory system. Its normal diameter ranges from 1.5 to 2.2 cm, depending on a person’s size and gender.
When the aorta dilates beyond 3 cm, this condition is referred to as an “abdominal aortic aneurysm” (AAA). This occurs when the aorta becomes weakened for various reasons. Most small aneurysms do not cause any symptoms and are often discovered incidentally.
Aneurysms smaller than 5 cm are considered low risk and are typically monitored with annual ultrasound scans. Repairing an aortic aneurysm is generally not recommended until the risk of rupture surpasses the risk associated with surgery. This threshold usually occurs at 5 cm in women and 5.5 cm in men [1].
Restriction on Driving
It’s important to note that in Australia, once an aneurysm exceeds 5.5 cm, there may be restrictions on your ability to drive.
What Happens to a Small Abdominal Aortic Aneurysm (AAA) Over Time
Over time, the stress on the weakened wall of the blood vessel can cause an aneurysm to grow, typically at a rate of about 1-2 mm per year. However, this growth rate can be accelerated by certain risk factors, particularly smoking. If an aneurysm grows more than 5 mm within a six-month period, it is considered rapidly expanding and may warrant intervention.
Risk Factors
While not all risk factors can be controlled, there are measures you can take to reduce the risk of rupture, slow the rate of aneurysm growth, and improve your overall health in preparation for surgery.
- Smoking: Smoking is the most significant risk factor for developing an AAA, with 75% of patients having a history of smoking. It is associated with a faster rate of aneurysm growth and an increased risk of rupture.
- High Blood Pressure (Hypertension): Having high blood pressure doubles the risk of developing an aneurysm and also increases the rate of its growth.
- Age: The likelihood of developing an aneurysm increases with age. Aneurysms are found in 1.7-3.3% of people over the age of 65.
- High Cholesterol Levels (Hypercholesterolemia): Elevated cholesterol levels are linked to a faster growth rate of aneurysms. Statins, a class of cholesterol-lowering medications, have been found to slow aneurysm growth, even in individuals with normal cholesterol levels. Additionally, statins reduce the risk of cardiovascular complications by 22% in patients with aneurysms.
- Gender: Men are four times more likely to develop an aneurysm than women.
- Family History: Individuals are up to three times more likely to have an aneurysm if a first-degree relative has had one.
Elective Treatment of Abdominal Aortic Aneurysm (AAA)
When it comes to treating an AAA, there are two main options: open surgery and endovascular (minimally invasive) repair. The choice between these procedures is based on several factors, including your age, existing health conditions, and personal preferences, all with the goal of achieving the best possible outcome.
The decision will also depend on the specific anatomy of the aneurysm, as not every treatment method is suitable for all patients. Together, we will consider your overall health, any allergies, and your tolerance for certain procedures.
Long-term outcomes for both open and endovascular repairs are quite similar, but there are important differences between the two options that you should be aware of.
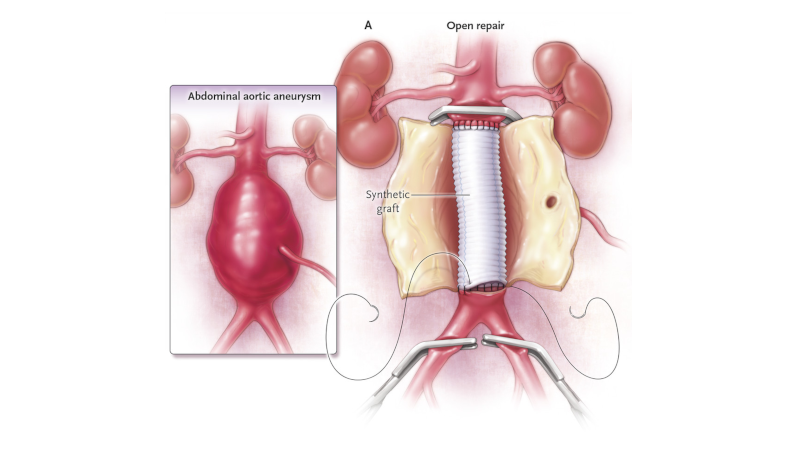
Open Surgery
Open surgery involves making an incision in the abdomen, either vertically or horizontally.
The purpose of this procedure is to replace the diseased section of the aorta with a prosthetic graft, typically made from Dacron. This graft is sewn onto the healthy part of the aorta, effectively taking over its function while the weakened section is replaced. The aneurysm sac is wrapped around the graft to serve as a barrier between it and the rest of the body, although it no longer bears the strain from the heart.
This procedure generally places more strain on the body, requiring most patients to spend 1-2 days in the Intensive Care Unit (ICU) and then an additional 7-10 days in the hospital.
One of the advantages of open surgery is that it typically requires less follow-up care in the future, allowing you to return to normal life without the need for frequent scans and ultrasounds after the initial recovery period. The risk of needing further interventions is generally lower compared to endovascular surgery.

Endovascular Aortic Aneurysm Repair (EVAR)
Endovascular repair is a minimally invasive procedure where a stent is inserted into the aorta through the femoral arteries in the groin. The stent is guided into place using X-ray imaging and contrast dye, and once in the correct position, it is expanded to exclude the aneurysm from blood flow.
The stent reinforces the aorta, redirecting blood flow and pressure through the stent rather than the weakened vessel, which helps prevent rupture.
After this surgery, most patients spend one night in the ICU and another 1-2 days in the hospital.
Endovascular surgery does require regular follow-up because there is a slightly higher chance that additional procedures may be needed, usually performed through the groin as well.
An endoleak can occur if blood continues to fill the aneurysm sac, often from small vessels in the spine. Occasionally, the graft may shift or kink, but most cases can be managed with monitoring rather than intervention. It’s crucial that you commit to yearly ultrasound scans for medium to long-term monitoring.
Although this is a newer technique, over 80% of aneurysm surgeries in Australia are now performed using this method.
Pros and Cons of Endovascular Aortic Aneurysm Repair (EVAR)
Although this is a newer technique, over 80% of aneurysm surgeries in Australia are now performed using this method.
Pros
- Lower risk of major complications: EVAR typically has a lower risk of serious complications during surgery compared to open surgery.
- Faster recovery: Patients are generally able to return to work and normal activities more quickly.
- Shorter hospital stay: Most patients spend fewer days in the hospital.
- Smaller incisions: The procedure involves smaller cuts, which can mean less pain and quicker healing.
- Quicker procedure: EVAR is typically a shorter surgery compared to open repair.
Cons
- Risk of endoleak: There is a possibility that blood may still enter the aneurysm sac, requiring further treatment.
- Ongoing monitoring: Regular scans, usually once a year, are needed to monitor for endoleaks or other complications.
- Use of contrast dye: The procedure requires the use of contrast dye, which can be a concern for patients with kidney issues.
What Can I Do About My AAA in the Meantime?
While an aneurysm cannot be reversed once it has developed, there are several steps you can take to slow its growth and improve your overall health in preparation for potential surgery:
Risk Management
Quit Smoking
Stopping smoking is the most important step you can take. It not only reduces the risk of the aneurysm rupturing and slows its growth but also improves your overall fitness for surgery. Both open and endovascular repairs require a general anesthetic, and being smoke-free helps your lungs and body handle the procedure better.
Medication
Taking prescribed medications such as statins, blood pressure medications, and aspirin can help manage your aneurysm. These medications work to lower cholesterol, control blood pressure, and reduce the risk of heart complications.
Stay Active
Regular physical activity helps maintain cardiovascular health and improves your ability to tolerate surgery. Simply going for a walk can make a significant difference in your overall fitness.
Weight Management
If you’re overweight, losing weight can ease the surgical process by providing better access to blood vessels and reducing the risk of complications. Additionally, a healthy weight aids in a smoother recovery.
Healthy Diet
A balanced diet, rich in nutrients, supports better surgical outcomes. Maintaining normal protein and albumin levels is essential, as these are critical for the body’s healing process.
Note
If you ever have concerns about the aneurysm, have severe abdominal or back pain it is important you seek immediate medical attentions.
Advice to GPs
What Can I Do for My Patient?
- Blood Pressure Control: Current guidelines recommend controlling blood pressure, and considering statins and antiplatelet therapy for all patients with AAA [1].
- Statins: Statins have been shown to reduce the growth rate of aneurysms, lower the risk of rupture, and decrease cardiovascular mortality when started at least 4 weeks before surgery [2].
- Antiplatelet Monotherapy: Aspirin or clopidogrel does not increase the risk of excessive bleeding, even before open surgery. These medications have been shown to improve perioperative and postoperative cardiovascular outcomes. If a patient is on dual antiplatelet therapy, it should not be discontinued, and endovascular aneurysm repair (EVAR) can still be considered [3].
- Smoking Cessation: Smoking is one of the most critical risk factors to address, as it provides the most significant benefit to the patient. Evidence shows that smokers are three times more likely to develop an aneurysm [4]. Smoking also increases the growth rate of aneurysms by up to 0.35 mm/year and raises the risk of rupture [5]. The benefits of smoking cessation, particularly in the perioperative period, are well-established across all types of surgery.
- Hypertension Management: Blood pressure control is essential. Lowering systolic blood pressure from 180 mmHg to 120 mmHg can reduce the rate of rupture by 66%. Controlling blood pressure also improves overall cardiovascular risk, with ACE inhibitors being slightly favored as the drug of choice for suitable patients [6].
- Family Screening: Guidelines recommend that any first-degree family member over the age of 50, whether male or female, should have an ultrasound scan every 10 years to rule out AAA. Studies suggest that a family history of AAA is associated with a faster aneurysm growth rate [7].
- Popliteal Pulses: If you detect prominent popliteal pulses, consider an ultrasound to check for a popliteal aneurysm. Approximately 10% of patients with an abdominal AAA also have a popliteal aneurysm [8].
- Reassurance: For aneurysms under 5 cm, the risk of rupture is extremely low. For instance, a 3.0 cm aneurysm carries an annual rupture risk of only 0.005% in men and 0.02% in women. We monitor aneurysms yearly to check for growth and ensure there are no concerning features.
Discovered an Incidental AAA in a Patient?
Abdominal aortic aneurysms (AAA) are often discovered incidentally during imaging. If your patient has reported symptoms such as back pain, abdominal pain, or groin/loin pain, and an aneurysm is detected on a CT angiography (CTA), they require urgent review by a vascular surgeon—either in the public or private sector. These patients should be transported to the emergency department by ambulance and should not drive themselves.
Aneurysms smaller than 5 cm have a very low risk of rupture. Asymptomatic aneurysms under 5 cm should be monitored yearly with an ultrasound and a clinical review. It’s important to note that an aneurysm larger than 5.5 cm may result in driving restrictions for both private and commercial licenses.
1. Dalman, R. L. (2019). The 2019 update of the European abdominal aortic aneurysm guidelines. Journal of Vascular Surgery, 69(3), 633-634.
2. H Wemmelund, A Høgh, H H Hundborg, R W Thomsen, S P Johnsen, J S Lindholt, Statin use and rupture of abdominal aortic aneurysm, British Journal of Surgery, Volume 101, Issue 8, July 2014, Pages 966–975, https://doi.org/10.1002/bjs.9517
3. S S Bahia, A Vidal-Diez, S R K Seshasai, I Shpitser, J R Brownrigg, B O Patterson, K K Ray, P J Holt, M M Thompson, A Karthikesalingam, Cardiovascular risk prevention and all-cause mortality in primary care patients with an abdominal aortic aneurysm, British Journal of Surgery, Volume 103, Issue 12, November 2016, Pages 1626–1633, https://doi.org/10.1002/bjs.10269
4. Jahangir E, Lipworth L, Edwards TL, et al. Smoking, sex, risk factors and abdominal aortic aneurysms: a prospective study of 18 782 persons aged above 65 years in the Southern Community Cohort Study J Epidemiol Community Health 2015;69:481-488.
5. M J Sweeting, S G Thompson, L C Brown, J T Powell, on behalf of the RESCAN collaborators, Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms, British Journal of Surgery, Volume 99, Issue 5, May 2012, Pages 655–665, https://doi.org/10.1002/bjs.8707
6. Kobeissi, E., Hibino, M., Pan, H., & Aune, D. (2019). Blood pressure, hypertension and the risk of abdominal aortic aneurysms: a systematic review and meta-analysis of cohort studies. European journal of epidemiology, 34, 547-555.https://doi.org/10.1002/bjs.10269
7. Verloes, A., Sakalihasan, N., Koulischer, L., & Limet, R. (1995). Aneurysms of the abdominal aorta: familial and genetic aspects in three hundred thirteen pedigrees. Journal of vascular surgery, 21(4), 646-655.
8. Diwan, A., Sarkar, R., Stanley, J. C., Zelenock, G. B., & Wakefield, T. W. (2000). Incidence of femoral and popliteal artery aneurysms in patients with abdominal aortic aneurysms. Journal of vascular surgery, 31(5), 863-869.https://doi.org/10.1002/bjs.9517